Ikigai: one’s reason for being and how I found mine
Too busy to read or prefer audio? Listen to the audio version of this blog below. Now available on my Spotify podcastFive years ago, I experienced the most extreme anti-climax. Following six months of intensive, gruelling studying and coaching by senior colleagues, I smashed the hardest exams of my life on my first attempt-the MRCOG. The MRCOG is the professional board examination for UK practising obstetricians and gynaecologists. You cannot progress in training or become a consultant(attending) without achieving the MRCOG. In 2018 I proudly became a member of the RCOG, celebrating alongside my pals Viner and Gary(pictured below). Our graduation was fantastic! The only person more relieved than myself that day was my poor husband, who had coped with an absent wife for six months.
(Left to right) Gary, Viner and I at our MRCOG graduation, London 2018
At the end of it all, I recall being sat on the train back to Edinburgh and thinking,“ Now what?” This feeling of anti-climax was accompanied by confusion and languishing. I knew the next step was to progress through advanced speciality training. I planned on focusing on early pregnancy, acute gynaecology and advanced labour ward practice. Whilst I found hospital medicine exciting and rewarding, I couldn’t quite see the big picture. Something was missing.
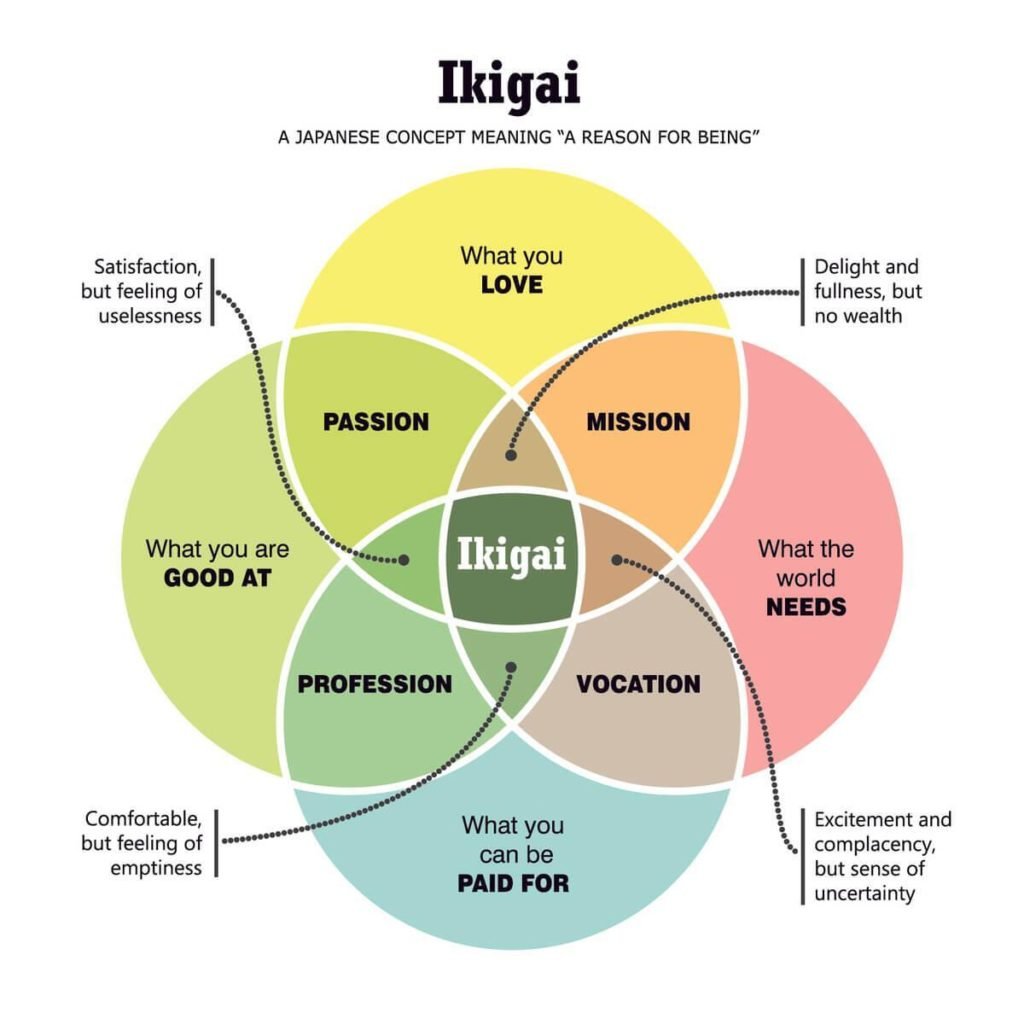
Our ikigai is what drives us- why we wake up in the morning and do whatever we do. It motivates us beyond the responsibilities, societal expectations, authorities and negative emotions that may also drive us.
Obstetrics & gynaecology is a seven-year run-through specialist training program. The downside of a run-through clinical training program is that without a natural built-in career break, it is possible to progress without thinking critically about one’s personal and wider career development. Without the right mentorship and sponsorship, it is easy to fall into the trap of jumping over career hurdles simply because it is ahead of you. Suddenly you are a consultant obstetrician & gynaecologist without a clear understanding of why you do what you do day in and day out.
When searching for your ikigai, you must answer four questions:
What do I love?
What am I good at?
What does the world need?
What can I be rewarded( paid for)?
The sweet spot where these four circles overlap is where you may find your ikigai.
I am passionate about global women’s health. This is likely because of my lived experience as a global citizen. Global health is frequently misunderstood to be healthcare only in low-resource settings in African, Asian and Latin American countries. However, the ongoing impact of migration, climate change and, more recently, the COVID-19 pandemic continue to remind us that we all live and work in resource-limited settings.
Therefore global health is better thought of as the business of reducing inequities within and between countries. Inequities exist globally in Nigeria, India, Brazil and Scotland.
Graphics by isi_designs
The COVID-19 pandemic put a spotlight on chronic health inequities amongst racially minoritised people. Three years into the pandemic with significant strains on the NHS, there has never been a greater need for health systems that proactively tackle inequities- disparities that are preventable, unfair and unjust. Beyond the social justice argument, there is a strong economic, cost-effectiveness and health quality argument for addressing variation in outcomes. These variations cost health systems billions annually. Inequalities cost the NHS £4.8 billion annually! We owe it to the workforce, patients and their families to consider additional factors which influence the quality and impact of whatever prescription or surgical procedure we deliver in a hospital.
In Scotland, I noticed patterns in health inequities- the same groups of people seemed to have worse outcomes. Sometimes they were described as marginalised or vulnerable. The same group were also labelled as “repeat” or “late attenders”, “ non-compliant”, or “difficult to reach”. Negative outcomes became normalised and almost expected. I noticed that in hospitals, we scrutinised individuals’ “bad health” choices but rarely critiqued or interrogated systemic factors that took away choice, acting as structural barriers to good health from these so-called vulnerable and marginalised groups.
I recall feeling uncomfortable with the realisation of my current limitations as a hospitalist to address deeply rooted structural issues that I now appreciated would continue to limit the outcome of whatever prescription or surgical treatment we provided in the hospital. I felt like I was engaging in an exercise of patching over cracks but wanted to be involved in preventing the cracks.
This is where I found my ikigai in appreciating the impact of social determinants of health (SDH) on variation in health outcomes. Most health workers have become familiar with the concept of SDH. But it is not uncommon to think that addressing SDH should remain squarely in the realm of public health- prevention, promotion, protection, and not acute care. It is surprising how divorced public health teaching is from medical education.
So, I went back to school to advance my knowledge and skills in public health, research methodology, and community co-production. And now, I am committed to addressing unwanted preventable variations in health outcomes by combining my multiple hats as a clinician and community organiser involved in community-based participatory research, which informs policy specifically aimed to eradicate health inequities for Black women living in Scotland. This is my mission statement and a core part of my ikigai.
I believe it is critical to find our ikigai because it is the key to finding joy in whatever you choose to do.
The Institute of Healthcare Improvement (IHI) state that joy in work promotes wellbeing, healthcare quality and patient safety.
Finding one’s ikigai is an important part of human existence and the key to achieving self-actualisation, the pinnacle of Maslow’s hierarchy of human needs. In the current climate of global workforce strains, it may be a way to address the crises of burnout and attrition.
So how can you find yours?
In finding my ikigai, I firmly reject the superficial, saccharine, toxic positivity definition of happiness. Ikigai is something deeper and more stable. Our ikigai is something deeper that belongs to us, is done voluntarily and brings joy.
Graphics by isi_designs
If you are still struggling to complete the circle, ask one close family member, friend, and work colleague ( 3 people) to complete the following sentences about you:
1. I have seen you at your happiest when…
2. I have seen you at your most fulfilled( alive) when…
3. If I was not a x( current career), you could imagine me being….
4. In 10 years time, what would you guess that I was up to?
5. My number one strength is…
6. My number one weakness is…
Chasing your ikigai can be scary and lonely, so find a community of like-minded people. Be brave. You will likely be told explicitly and implicitly that you cannot do “xyz..”. You may be warned that some of your choices will hamper your career progression. We live in a world where people are anaesthetised by overwork, social media and sugar. Deciding on something other than what is considered the norm will make you stand out. Your actions may trigger negative emotions in people around you. Expect some resistance and surround yourself with a good support system that will energise and inspire you to continue moving forward. Remember, joy is a long game.
Lean into that support when you receive rejection and caution. When you do succeed, bravely share your story to inspire others.
I have survived and thrived in spaces where I am considered the oddball not solely because of my personal ability- but because I have found and held on to my ikigai. I am “being” and “doing” bravely in a community of like-minded individuals.
That’s my secret sauce!
P.S
In future blogs, I may share my reflections on how hospitalists and non-public health practitioners may engage meaningfully in addressing the impact of social determinants of health (SDH) in acute settings through quality improvement( QI), audit, research, significant adverse event reviews ( SAER) and equality, diversity & inclusion training.
Maybe I’ll call it “ Help, which social determinant of health should I address in my 15-minute consultation?”
What do you think?
P.S
As always, if my thoughts this week struck a cord, piqued your interest, or you’d like to explore some of these ideas further or have questions, leave a comment and write to me HERE.